Ulnar neuropathy after removal of contraceptive pill
A case of ulnar nerve neuropraxia after an attempted removal of a subdermal contraceptive implant is presented
Dr Louise Fitzgerald, Plastic Surgery SHO, Beaumont Hospital, Dublin, Dr Jeffrey CY Chan, Plastic Surgery SPR, Department of Plastic, Reconstructive and Hand Surgery, Beaumont Hospital, Dublin, Dr Laura Kearney, Plastic Surgery Registrar, Department of Plastic, Reconstructive and Hand Surgery, Beaumont Hospital, Dublin and Dr Nadeem Ajmal, Plastic Surgery Consultant, Department of Plastic, Reconstructive and Hand Surgery, Beaumont Hospital, Dublin
February 4, 2016
- Article
- Similar articles
-
Implantable hormonal contraceptive devices are an effective, economical and convenient method of reversible long-term contraception. The insertion and subsequent removal are relatively uncomplicated once the upper arm anatomy is appreciated. While ulnar nerve injury has previously been described with Norplant, this has not been reported with Implanon. We present a case of a 30-year-old with ulnar nerve neuropraxia after an attempted removal of Implanon. We discuss the method of insertion and removal of the device, review the literature for reported cases of peripheral nerve injuries and recommended alternative insertion sites.
Case report
A 30-year-old right hand dominant woman was referred to our unit after her general practitioner attempted to remove the Implanon from the medial aspect of her left mid-arm. The patient presented with paraesthesia and clawing of her little and ring fingers. There was weakness of fingers abduction and adduction, and Froment’s sign was positive. Wartenberg’s sign was not present. The Implanon was not clinically palpable but there was minor bruising surrounding the incision.
An ultrasound scan revealed the location of the Implanon. Surgical exploration under general anaesthesia was performed to examine her ulnar nerve and to retrieve the implant which was found under the triceps muscle fascia intramuscularly. The ulnar nerve had a normal macroscopic appearance (see Figure 1) and was surrounded with rather unimpressive localised haematoma and muscle bruising, supporting a diagnosis of ulnar nerve neuropraxia. Her postoperative course was uneventful. Occupational therapy and physiotherapy were commenced to address clawing of her little and ring fingers. While motor function has now improved four months following surgery, her sensory symptoms have not subjectively improved.
 Figure 1. The ulnar nerve had a normal macroscopic appearance and was surrounded with rather unimpressive localised haematoma and muscle bruising, supporting a diagnosis of ulnar nerve neuropraxia(click to enlarge)
Figure 1. The ulnar nerve had a normal macroscopic appearance and was surrounded with rather unimpressive localised haematoma and muscle bruising, supporting a diagnosis of ulnar nerve neuropraxia(click to enlarge)
Discussion
Anatomy10
The compact, dense brachial fascia encloses the muscles of the upper arm. The subcutaneous vessels, nerves, and the lymphatic vessels are vulnerable to damage in their superficial location. Ulnar nerve comes from the medial cord of the brachial plexus (C8-T1). In the arm it lies posteromedial to brachial artery in anterior compartment of upper half arm. It pierces the medial IM septum at the arcade of Struthers approximately 8cm from medial epicondyle and lies medial to the triceps. The arcade of Struthers is an aponeurotic band extending from the medial IM septum to the medial head of the triceps.
The ulnar nerve innervates the skin of the fifth digit and the medial half of the fourth digit, and the corresponding part of the palm. The ulnar nerve and its branches innervate muscles in the forearm and hand. Clinically, nerve injuries may lead to:
Motor deficit – characterised by a weakness in flexion of the hand at the wrist, loss of flexion of ulnar half of digits, or the 4th and 5th digits, loss of ability to cross the digits of the hand. The presence of a claw hand deformity when the hand is at rest is due to hyperextension of the fourth and fifth digits at the meta carpophalangeal joints and flexion at the interphalangeal joints.
Sensory deficit – loss of sensation or paraesthesia in ulnar half of the palm and dorsum of hand, and medial 1.5 digits on both palmar and dorsal aspects of the hand.
The device
Implanon is a single-rod contraceptive implant2 consisting of a core containing the selective progestin etonogestrel and ethylene vinyl acetate (EVA) copolymer surrounded by a rate-controlling EVA membrane. The rod is 40mm in length and 2mm in diameter. The reported incidence of complications from its insertion (0.3%) and removal (0.2%) is low.2,6
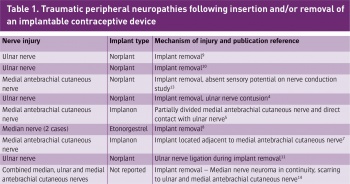
Injuries to peripheral nerves from insertion or removal of Implanon have been previously documented in the literature (Table 1) and have led to litigations.4,5 Wechselberger et al and Brown et al reported injuries to the medial cutaneous nerve of the forearm associated with Implanon.5,7 Spinner et al reported on a combined median, ulnar and medial antebrachial cutaneous nerves injuries, while Gilles et al reported two cases of median nerve injuries.8 Other authors had previously reported injuries to the ulnar nerve associated with Norplant.4,9,10,11 Norplant, an older generation of subdermal contraceptive implant, consisted of a set of six subdermal rods therefore proportionally increasing the size of implantation area and risk.
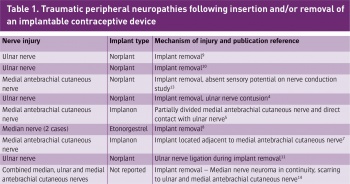
(click to enlarge)
 Figure 1. The ulnar nerve had a normal macroscopic appearance and was surrounded with rather unimpressive localised haematoma and muscle bruising, supporting a diagnosis of ulnar nerve neuropraxia(click to enlarge)
Figure 1. The ulnar nerve had a normal macroscopic appearance and was surrounded with rather unimpressive localised haematoma and muscle bruising, supporting a diagnosis of ulnar nerve neuropraxia(click to enlarge)